PCOS (Polycystic Ovary Syndrome)
PCOS is a common but often confusing condition that can affect your hormones, cycles, ovulation, and overall wellbeing. Symptoms such as irregular periods, acne, excess hair growth, or difficulty conceiving can feel overwhelming, but gaining clarity is an important first step. Through thoughtful assessment and personalised care, I help you understand your hormonal patterns and create a tailored plan that supports symptom control, cycle regulation, metabolic health, and long-term fertility—so you can feel more balanced, informed, and supported.
“Exploring and understanding PCOS is a step toward rediscovering balance, supporting your health, honouring your body, and moving forward with confidence and ease.”
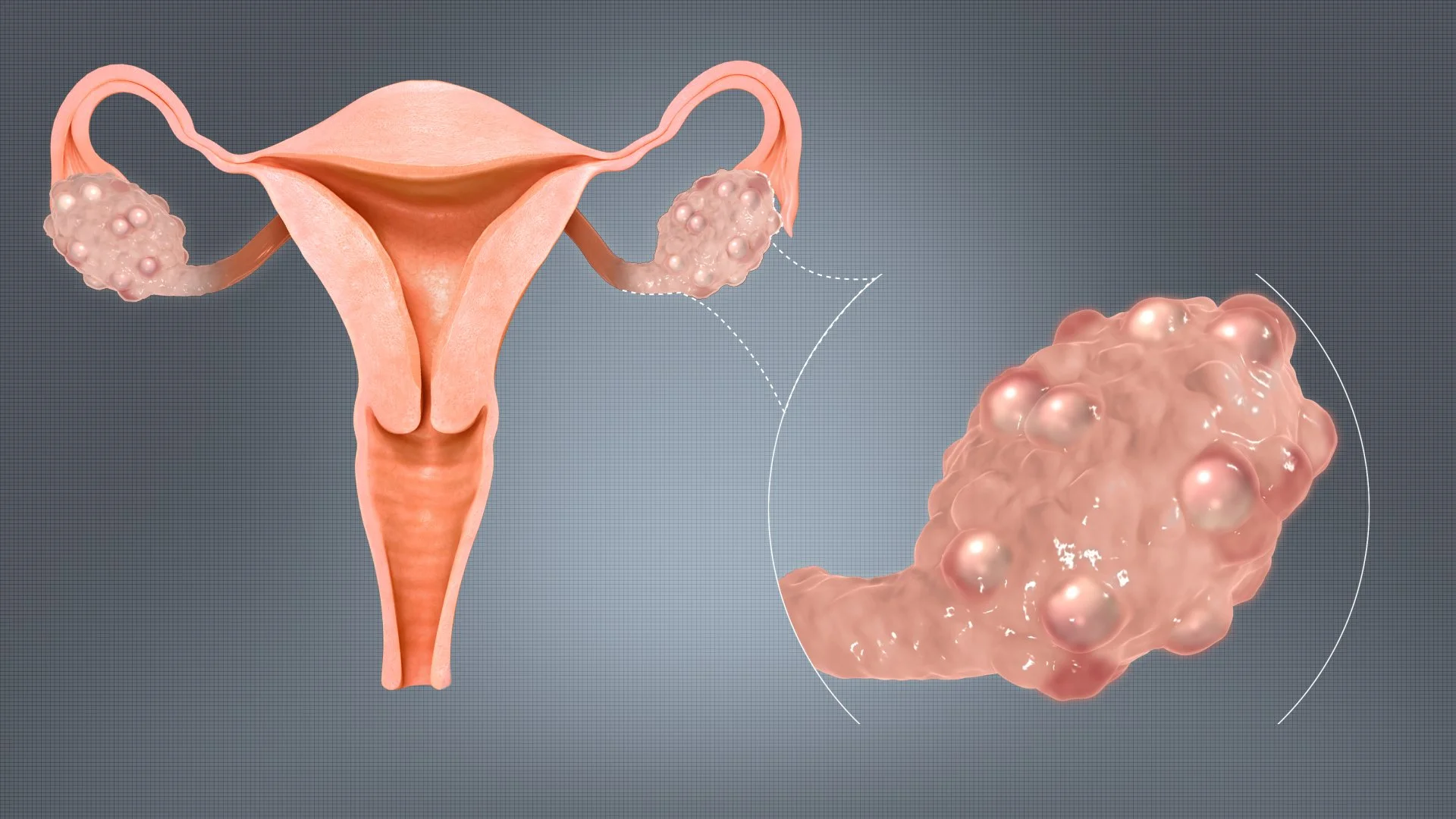
Understanding PCOS
PCOS is a complex endocrine condition with reproductive, metabolic and psychological dimensions. Management requires comprehensive assessment across multiple body systems, guided by international PCOS guidelines.
PCOS typically involves:
Ovulatory dysfunction (irregular or absent ovulation)
Androgen excess (acne, hair growth, elevated testosterone)
Polycystic ovarian morphology
Symptoms vary widely, making personalised care essential.
Diagnostic Accuracy Is Key
Diagnosis follows Rotterdam/International guidelines and includes:
Detailed cycle history
Biochemical androgens (testosterone, SHBG, free androgen index)
Ovarian ultrasound (international cut-offs)
Exclusion of mimicking disorders (thyroid dysfunction, hyperprolactinaemia, CAH)
Metabolic screening
Hormonal Management
Cycle Regulation
For symptom control or endometrial protection.
Hormonal options:
Combined pill
Progesterone-only methods
Cyclical progesterone
Non-hormonal
Nutritional support - dietary changes, inositol
Regular aerobic exercise
Hyperandrogenism Management
OCP
Anti-androgens (spironolactone, cyproterone - with appropriate contraception)
Dermatology input when required
Metabolic Health & Insulin Resistance
Metabolic assessment includes:
Fasting glucose
OGTT (gold standard in PCOS)
Lipid profile
Blood pressure
Body composition
Evidence-based lifestyle interventions focus on:
Resistance and aerobic training
Structured nutritional strategies (Mediterranean-style patterns preferred)
Sleep and stress optimisation
Metformin may be recommended for:
Impaired glucose tolerance
Insulin resistance
Adjunct to ovulation induction
Fertility in PCOS
Ovulatory dysfunction is a common driver of subfertility, and outcomes with treatment are excellent.
Options include:
Ovulation induction (Letrozole first-line; Clomiphene second-line)
IUI in selected couples
IVF when induction is unsuccessful or other factors coexist
Ovarian drilling is rarely used; laparoscopy is considered only in select circumstances
Individualised ovarian stimulation to minimise risk of OHSS
Fertility considerations
Monitoring protocols are tailored to reduce OHSS
Trigger choice (agonist vs hCG) is carefully selected
Freeze-all cycles may be used in high-risk responders
Weight-neutral fertility support models are prioritised
Mental Health in PCOS
PCOS is associated with:
Higher rates of anxiety and depression
Body image concerns
Increased disordered eating risk
This is incorporated into care through supportive counselling and multidisciplinary input when needed.



