In Vitro Fertilisation (IVF)
IVF is one of the most transformative and hopeful paths in fertility care - a journey that blends science, preparation, and emotional support. The steps leading up to IVF offer a valuable opportunity to optimise reproductive health, support egg and sperm quality, and improve your chances of a healthy pregnancy. My aim is to guide individuals and couples through every stage of the IVF process with clarity, compassion, and evidence-based care - helping you feel informed, supported, and empowered at every step.
“IVF is a reminder that families are built not just through biology, but through courage, intention, and hope. It’s a chance to support your body, honour your story, and move forward with possibility.”
What is IVF?
In-vitro fertilisation (IVF) involves stimulating the ovaries to produce eggs, retrieving those eggs, fertilising them in the lab, and transferring one or more embryos into the uterus, with the hope of achieving pregnancy. Over the years, this process has evolved into a highly refined series of steps, each optimised to give you the best chance of success.
Is IVF right for me?
IVF is often considered when simpler fertility treatments (such as ovulation induction or intrauterine insemination - IUI) have not succeeded or are unlikely to be effective. Common indications include:
Tubal disease or blocked fallopian tubes
Severe male factor infertility
Endometriosis or uterine abnormalities
Advanced maternal age or diminished ovarian reserve
Unexplained infertility
Same-sex couples or single individuals wishing to conceive
Genetic conditions requiring preimplantation testing
Before recommending IVF, we perform a comprehensive diagnostic workup - on you and your partner - to clarify underlying issues and guide a personalised plan. This ensures you only pursue an IVF cycle when it truly offers benefit.
Our IVF process - step by step
Here’s a general outline of how an IVF cycle usually unfolds:
Diagnostic assessment prior to considering IVF
Blood tests (Antenatal screen, hormonal assessment)
Imaging/ultrasound of ovaries and uterus
Semen analysis
Genetic screening when indicated - genetic carrier screening, consider extended carrier screen and karyotype.
Additional investigations (e.g. laparoscopy, hysteroscopy) if structural issues or endometriosis is suspected. Discuss if this is something that is relevant for you.
Ovarian stimulation
Hormonal medications are used over ~10-14 days to stimulate multiple follicle development. We closely monitor your response with ultrasounds and hormone testing. The choice of medication will be tailored to your individual circumstances as will the dose, these are usually injections.Egg retrieval
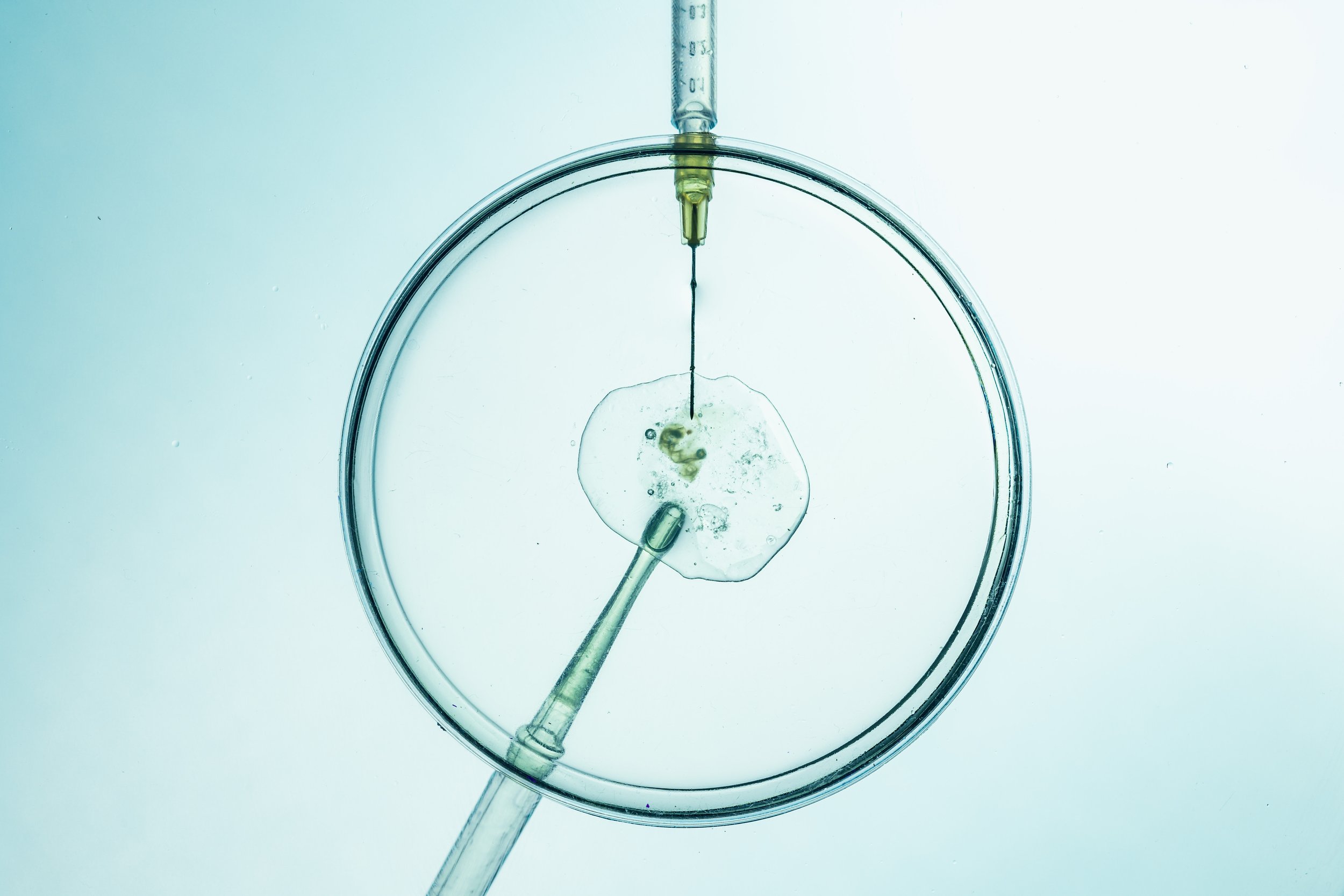
Under sedation (light anaesthetic), eggs are retrieved via a minimally invasive transvaginal procedure (usually ~30 minutes)Fertilisation & Embryo culture
Eggs are fertilised in the embryology lab. Embryos are cultured (often to the blastocyst stage), and selected for transfer. We may offer ICSI (intracytoplasmic sperm injection) in cases of male factor infertility.IVF - allows natural selection of the sperm to fertilise the egg
ICSI - the scientists choose a single sperm and inject directly into the egg. During this procedure the egg is prepared for injection - by removing the cumulus cells.
Embryo transfer
A short procedure (about 10 minutes) to place embryos into your uterus-usually without anaesthesia. It is performed under ultrasound guidance - this is a transabdominal scan. So you need a full bladder.Luteal support and pregnancy test
Hormonal support continues while the embryo attempts implantation. A blood pregnancy test follows ~9-14 days after transfer.Follow-up & next steps
Whether the cycle succeeds or not, we review outcomes with you, adjust protocols, and plan future steps or alternative strategies (such as frozen embryo transfer, donor eggs, or surrogacy if needed).
Why choose us?
Personalised care
I believe each patient deserves an individualised treatment plan, not a “one size fits all” approach.Transparent advice
I am committed to providing honest guidance about your likelihood of success, potential risks, and alternative pathways. And believe in the principle of giving realistic counsel.Scientific excellence
The protocols and laboratory techniques used are grounded in the latest evidence and best practices. We constantly review outcomes and refine our methods.Emotional and holistic support
I understand fertility treatment is more than medical-it touches your heart, your identity, and your hopes. Our team supports you with empathy, psychological care, and clear communication.Inclusive care
Regardless of your relationship status, sexuality, identity, or background, you are welcome here. We provide fertility pathways for single individuals, LGBTQIA+ couples, and those considering donor or surrogacy options.
Costs & financial transparency
Fertility treatments, especially IVF, involve multiple cost components (medications, scans, procedures, lab fees). We believe in upfront clarity and will provide you with a detailed estimate before you commit.
We will also help you understand Medicare rebates, private health fund coverages, and ancillary costs (e.g. genetic testing, fertility preservation).
Success rates & realistic expectations
Success in IVF depends on many factors-most importantly, your age and egg quality. While we strive to maximise your odds, there are no guarantees. We walk this journey together, always grounded in realistic, evidence-based counsel.
Success rates are shared with patients and contextualised (e.g. age brackets, fresh vs frozen embryos). Dr Rebecca Mackenzie-Proctor brings over a decade of experience and thousands of patient journeys to her practice, offering both scientific insight and compassionate perspective.


