Endometriosis
Endometriosis is a complex and often misunderstood condition that can affect your comfort, fertility, and overall wellbeing. Whether you’re experiencing pain, heavy periods, difficulty conceiving, or seeking clarity about your symptoms, gaining insight into endometriosis is an important step toward relief and control. Through careful assessment and personalised medical or surgical care, I’m here to help you understand your options and create a plan that supports both your immediate comfort and long-term reproductive health, with compassionate, evidence-based guidance throughout.
“Exploring endometriosis is a step toward reclaiming your comfort, your health, and your sense of ease in your body.”
Endometriosis Care
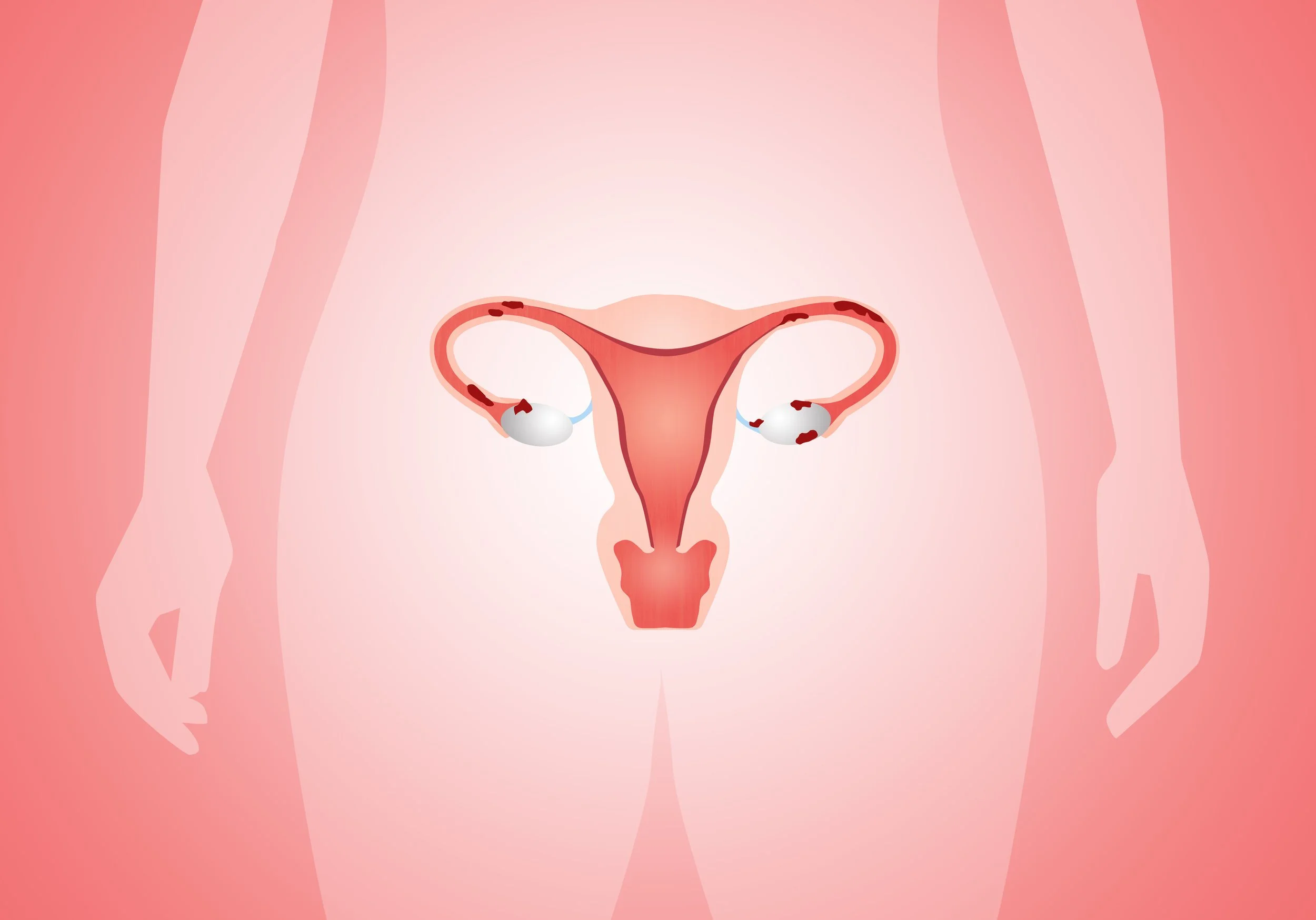
Endometriosis is a chronic inflammatory, hormonal and immune-mediated condition where tissue similar to endometrium grows outside the uterus. It can infiltrate the pelvis, ovaries, bowel, bladder, nerves, and beyond. It affects quality of life, fertility, pelvic function, emotional wellbeing and long-term health.
Dr Rebecca Mackenzie-Proctor provides contemporary, whole-person endometriosis care combining expert diagnosis, modern hormonal therapies, surgical precision and fertility-focused management.
Understanding Endometriosis
Endometriosis involves:
Inflammation and cytokine activation
Progesterone resistance and oestrogen dominance at lesion level
Altered immune response
Pelvic nerve involvement contributing to chronic pain
Adhesion formation and organ distortion
It commonly presents with:
Severe period pain
Pain with sex
Bowel/bladder symptoms
Chronic pelvic pain
Heavy periods
Fatigue
Infertility or difficulty conceiving
Symptom severity does not always correlate with disease stage—this is why careful assessment is essential.
Comprehensive Diagnostic Approach
Diagnosis includes:
Full menstrual and symptom mapping
Pain phenotype assessment
Endometriosis-focused pelvic ultrasound (transvaginal preferred)
Evaluation for adenomyosis
Preoperative fertility evaluation if appropriate
Ovarian reserve testing when clinically indicated (e.g., endometriomas)
Where deep infiltrating disease is suspected, collaboration with colorectal and urological surgical teams may be initiated.
Medical Management
Medical therapy aims to reduce pain, inflammation and hormonal stimulation of lesions. Options include:
• Hormonal therapies - not appropriate for fertility
Combined oral contraceptive pill (cyclical or continuous)
Progesterone-only pill
Levonorgestrel IUD
Dienogest (in appropriate patients)
Short-term GnRH analogues with add-back therapy
These treatments do not remove endometriosis, but can significantly improve symptoms.
• Adjunct therapies
Pelvic floor physiotherapy (gold standard for pain + dyspareunia)
Diet modifications (anti-inflammatory, low FODMAP when indicated)
Psychological and pain management tools
Acupuncture (supportive evidence for pain reduction)
Nutrition support for bowel involvement, energy, iron, and mood
Advanced Laparoscopic Surgery
Surgical excision remains the most effective method of removing endometriosis.
Dr Mackenzie-Proctor performs:
Precision excision of superficial + deep disease
Ovarian endometrioma cystectomy with ovarian tissue sparing
Adhesiolysis
Correction of pelvic anatomy
My surgical goals:
Remove disease safely
Restore anatomy
Preserve fertility
Minimise adhesions
Integrate postoperative medical therapy where beneficial
Endometriosis & Fertility
Endometriosis can impact fertility through:
Inflammation impairing egg quality
Altered endometrial receptivity
Tubal distortion or blockage
Ovarian reserve reduction in severe disease
Adhesions disrupting anatomy
Fertility strategies include:
Timed natural conception with ovulation optimisation
Laparoscopic excision - may improve outcomes for those with early stage endometriosis
Ovulation induction - limited evidence
IUI or IVF with personalised ovarian stimulation
Pre- and postoperative fertility counselling and support.
Dr Rebecca Mackenzie-Proctor takes a holistic, team-based approach to care, working closely with pain specialists, physiotherapists, and psychologists to support every aspect of your health and wellbeing. Some patients may benefit from surgery prior to IVF - for example, large endometriomas or significant deep disease-but this is always tailored.